Week 6: It's All In the Details + Musings From a Student on a Stool Gazing Longingly into the OR
Holly Zheng
4:22 PM
Greetings again!
I arrived at the hospital at 6:30 am yesterday morning ready to observe a Stage I DBS electrode placement operation. The residents were already bustling about when I walked into the pre-op rooms (apparently everyone is a morning person here). I was able to witness Dr. Kasoff attach a Leksell frame to a patient's head, which had a sad undertone to it. The patient's head was numbed under local anesthesia and the frame is attached via screws. Securing the metal rectangle looks extremely uncomfortable, and by the expression on the patient's face, he wasn't having the best time either.
The half circle apparatus isn't attached until the patient is in the OR. What the picture isn't showing is this plastic cage (the localizer) that is attached to the frame when the patient gets a pre-op CT scan.
Who knew it was so difficult to find images of extremely specific relatively new neurosurgery apparatuses?
After the pre-op CT scan, the patient is wheeled into the OR and the operation begins. Because I was not in the room during the procedure, I can't talk much on the details, but here is what I gathered:
1. The patient is 'asleep' at the beginning and end of the operation. That is, he/she is unconscious when the surgeon is making the incision, drilling the hole, and opening the dura (and closing). It makes a lot of sense because I think it would be extremely difficult to remain calm if I heard someone drilling into my skull. There is most likely a more scientific explanation to why the patient is unconscious and I will update this post if I out the reason.
2. The patient has to be awake when the electrode is being inserted to ensure that a desired clinical outcome is achieved. This ties into the whole debate of anatomy vs. physiology that I will expand on in a later post. If the tremor is still present, the surgeon often will do multiple runs with the electrode.
3. If the tremor is temporarily suppressed right after the electrode is inserted (without any electrical stimulation), that's a pretty good indication that the electrode is in a good spot.
4. Sometimes the patient will feel tingling when there is a current. Sometimes the tingling will disappear within a minute or two (this is good). If the tingling persists, the electrode needs to be adjusted because it is uncomfortable to the patient. Where the tingling is located gives the surgeon a pretty good idea how to adjust the electrode.
5. In addition to checking for tremor suppression, the doctors also check for slurred speech (or lack thereof) and the breadth of the visual field. The patients are asked to count backwards from 10, drink from an empty cup (no fluids before or during surgery!), and touch their finger to a doctor's moving hand.
6. After the electrode is inserted, the patient is asked to move around certain parts of his body (or have the doctors poke and prod at his body). If the electrode is in the correct position, you can actually hear these movements via neural noise. Neural noise is this static sound. For example, if you move your jaw, the static sound may start popping at a high frequency.
That's all I have to today. I wasn't even in the operating room and I was a bit exhausted trying to keep up with all the technical details (from the research papers). The entire operation was close to eight hours long. More posts are coming up about the setup of this project and some more background information that I still need to mention.
Phew! I hope I will be able to build up endurance by watching more and more of these surgeries (and not internally cry every time we take the stairs from the first floor surgery rooms to the offices on the fourth floor). My calf muscles have really been shaping up while I stand by the window of the OR. Compared to the ever chirpy doctors and nurses, I still have a long way to go (and many more cups of coffee to drink).
Holly
I arrived at the hospital at 6:30 am yesterday morning ready to observe a Stage I DBS electrode placement operation. The residents were already bustling about when I walked into the pre-op rooms (apparently everyone is a morning person here). I was able to witness Dr. Kasoff attach a Leksell frame to a patient's head, which had a sad undertone to it. The patient's head was numbed under local anesthesia and the frame is attached via screws. Securing the metal rectangle looks extremely uncomfortable, and by the expression on the patient's face, he wasn't having the best time either.
The half circle apparatus isn't attached until the patient is in the OR. What the picture isn't showing is this plastic cage (the localizer) that is attached to the frame when the patient gets a pre-op CT scan.
 |
| This (localizer) is attached to the Leksell frame when the patient gets a CT scan. This localizer provides axises for the surgeon to pinpoint his target. |
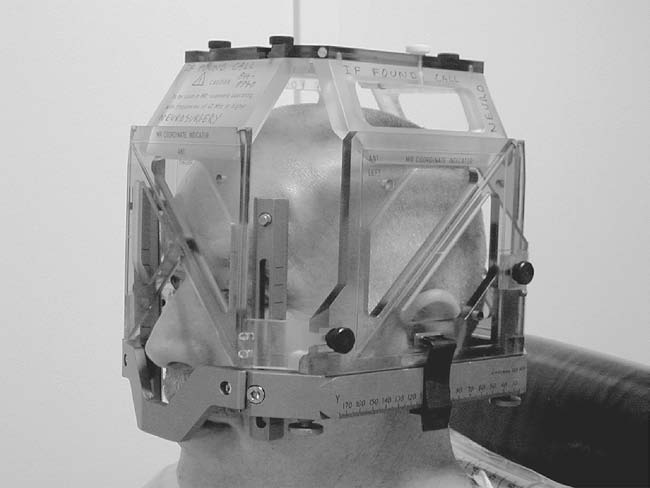 |
| A different localizer is used, but this is the general idea. |
After the pre-op CT scan, the patient is wheeled into the OR and the operation begins. Because I was not in the room during the procedure, I can't talk much on the details, but here is what I gathered:
1. The patient is 'asleep' at the beginning and end of the operation. That is, he/she is unconscious when the surgeon is making the incision, drilling the hole, and opening the dura (and closing). It makes a lot of sense because I think it would be extremely difficult to remain calm if I heard someone drilling into my skull. There is most likely a more scientific explanation to why the patient is unconscious and I will update this post if I out the reason.
2. The patient has to be awake when the electrode is being inserted to ensure that a desired clinical outcome is achieved. This ties into the whole debate of anatomy vs. physiology that I will expand on in a later post. If the tremor is still present, the surgeon often will do multiple runs with the electrode.
3. If the tremor is temporarily suppressed right after the electrode is inserted (without any electrical stimulation), that's a pretty good indication that the electrode is in a good spot.
4. Sometimes the patient will feel tingling when there is a current. Sometimes the tingling will disappear within a minute or two (this is good). If the tingling persists, the electrode needs to be adjusted because it is uncomfortable to the patient. Where the tingling is located gives the surgeon a pretty good idea how to adjust the electrode.
5. In addition to checking for tremor suppression, the doctors also check for slurred speech (or lack thereof) and the breadth of the visual field. The patients are asked to count backwards from 10, drink from an empty cup (no fluids before or during surgery!), and touch their finger to a doctor's moving hand.
6. After the electrode is inserted, the patient is asked to move around certain parts of his body (or have the doctors poke and prod at his body). If the electrode is in the correct position, you can actually hear these movements via neural noise. Neural noise is this static sound. For example, if you move your jaw, the static sound may start popping at a high frequency.
That's all I have to today. I wasn't even in the operating room and I was a bit exhausted trying to keep up with all the technical details (from the research papers). The entire operation was close to eight hours long. More posts are coming up about the setup of this project and some more background information that I still need to mention.
Phew! I hope I will be able to build up endurance by watching more and more of these surgeries (and not internally cry every time we take the stairs from the first floor surgery rooms to the offices on the fourth floor). My calf muscles have really been shaping up while I stand by the window of the OR. Compared to the ever chirpy doctors and nurses, I still have a long way to go (and many more cups of coffee to drink).
Holly

Post a Comment