Greetings again!
This post is a long time coming. I couldn't end this blog without some type of farewell and thank you to all of the people who have helped me on this incredible journey.
First off - the presentation. Thank you to everyone who came despite the fact it was a Saturday afternoon and the weather was bearable in terms of Tucson standards. I think I can speak for all of us who presented that day that it was so much fun sharing what we've been up to for the past few months. For anyone who is curious...the link to my presentation is below:
https://app.emaze.com/@ALLRRCTF/srp
I don't have many words on the slides, but I might upload my presentation notes for anyone who wants to get a basic just of my project without reading through the long (and frankly quite tedious) posts on this blog.
I am, of course, most grateful to Dr. Kasoff, my SRP mentor, for offering me (the incredibly inexperienced and unknowledgeable high liability high school student) this opportunity and seeing it through until the end. His schedule was always full, yet he still willingly took the time to answer my questions, meet with me to discuss my project, and allow me to shadow him while he treated his patients.
I originally began this project looking forward to OR time the most. To me, it was the coolest thing, being able to observe operations in the flesh (no pun intended) rather than watching through a computer screen via YouTube. Yet, after finishing this project, I found myself enjoying witnessing patient/doctor/nurse interactions more than anything. It's very cliche and expected - when treating patients, you are exposed to the stories of all these strangers, every one of them has an enthralling tale to tell. Cliche as it is, the stories are addicting, and you can't help but be captivated by each one. The elderly couple, both with walking impairments, both accompanying each other into surgery. The other couple in their mid sixties who still joke around like teenagers...
So I can say my biggest lesson wasn't the procedures I learned or the results of the many research papers I memorized. My biggest lesson was in patient care and bedside manners - lessons that cannot be taught by textbooks. Watching Dr. Kasoff, the various nurses, residents, and technicians treat the patients has been my most significant takeaway.
In fact, this entire project has broadened the scope of my understanding of the field of medicine. The term "teaching hospital" has taken on a new meaning. During the operation, various technicians, nurses, doctors, residents, and company representatives would approach me asking if I had any questions and enthusiastically answered all of them. It was a very positive environment that I am deeply grateful for. The staff members in the hospital were humble, patient, and occasionally unnecessarily sassy :)
Another thank you to the patients who I have seen who allowed me to tag along their DBS journey.
Participating in this project is a privilege. It is a privilege because I saw patients at their vulnerable state. I learned their name, their illnesses, their medical history, their bodies. I learned more about some patients than some of their closest friends know. It is a privilege to be trusted, and it is essential to abide by the morals of consent and confidentiality, to make them feel comfortable and safe.
To conclude, I must say thank you to the teachers of BASIS. To Mr. Kittredge for dealing with all of our grievances and frustrations, and encouraging a group of senioritis prone teenagers to keep our act together for at least a few months before college begins. To Mr. Johnston, my biology teacher and my SRP advisor, for teaching me biology, making fun of me in front of my classmates so I no longer have stage fright, and for dangling various dead insects and spiders in my face so I can appreciate not only human physiology but all aspects of biology. Thank you to all of my teachers at BASIS for possibly one of the best high school educations in the nation. Thank you for grounding me and motivating me to push my potential.
And here are pictures of us happy smiling seniors concluding Day 1 of our SRP presentations:
This post is a long time coming. I couldn't end this blog without some type of farewell and thank you to all of the people who have helped me on this incredible journey.
First off - the presentation. Thank you to everyone who came despite the fact it was a Saturday afternoon and the weather was bearable in terms of Tucson standards. I think I can speak for all of us who presented that day that it was so much fun sharing what we've been up to for the past few months. For anyone who is curious...the link to my presentation is below:
https://app.emaze.com/@ALLRRCTF/srp
I don't have many words on the slides, but I might upload my presentation notes for anyone who wants to get a basic just of my project without reading through the long (and frankly quite tedious) posts on this blog.
I am, of course, most grateful to Dr. Kasoff, my SRP mentor, for offering me (the incredibly inexperienced and unknowledgeable high liability high school student) this opportunity and seeing it through until the end. His schedule was always full, yet he still willingly took the time to answer my questions, meet with me to discuss my project, and allow me to shadow him while he treated his patients.
I originally began this project looking forward to OR time the most. To me, it was the coolest thing, being able to observe operations in the flesh (no pun intended) rather than watching through a computer screen via YouTube. Yet, after finishing this project, I found myself enjoying witnessing patient/doctor/nurse interactions more than anything. It's very cliche and expected - when treating patients, you are exposed to the stories of all these strangers, every one of them has an enthralling tale to tell. Cliche as it is, the stories are addicting, and you can't help but be captivated by each one. The elderly couple, both with walking impairments, both accompanying each other into surgery. The other couple in their mid sixties who still joke around like teenagers...
So I can say my biggest lesson wasn't the procedures I learned or the results of the many research papers I memorized. My biggest lesson was in patient care and bedside manners - lessons that cannot be taught by textbooks. Watching Dr. Kasoff, the various nurses, residents, and technicians treat the patients has been my most significant takeaway.
In fact, this entire project has broadened the scope of my understanding of the field of medicine. The term "teaching hospital" has taken on a new meaning. During the operation, various technicians, nurses, doctors, residents, and company representatives would approach me asking if I had any questions and enthusiastically answered all of them. It was a very positive environment that I am deeply grateful for. The staff members in the hospital were humble, patient, and occasionally unnecessarily sassy :)
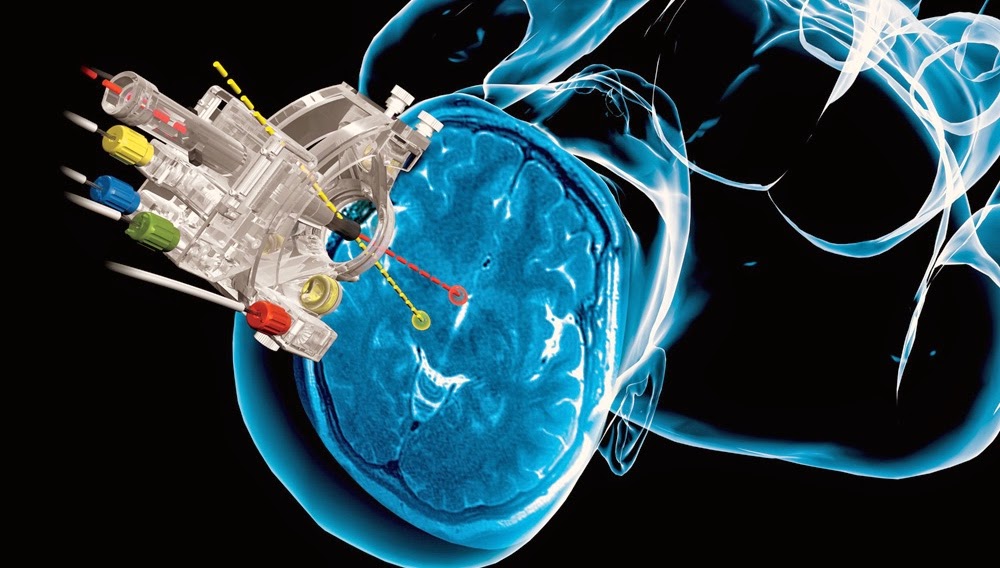
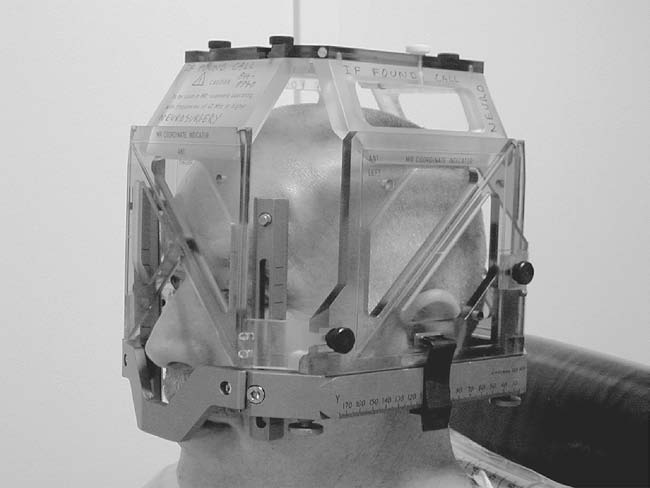
Another thank you to the patients who I have seen who allowed me to tag along their DBS journey.
Participating in this project is a privilege. It is a privilege because I saw patients at their vulnerable state. I learned their name, their illnesses, their medical history, their bodies. I learned more about some patients than some of their closest friends know. It is a privilege to be trusted, and it is essential to abide by the morals of consent and confidentiality, to make them feel comfortable and safe.
To conclude, I must say thank you to the teachers of BASIS. To Mr. Kittredge for dealing with all of our grievances and frustrations, and encouraging a group of senioritis prone teenagers to keep our act together for at least a few months before college begins. To Mr. Johnston, my biology teacher and my SRP advisor, for teaching me biology, making fun of me in front of my classmates so I no longer have stage fright, and for dangling various dead insects and spiders in my face so I can appreciate not only human physiology but all aspects of biology. Thank you to all of my teachers at BASIS for possibly one of the best high school educations in the nation. Thank you for grounding me and motivating me to push my potential.
And here are pictures of us happy smiling seniors concluding Day 1 of our SRP presentations:
Thank you for sticking with me through this journey! It's been the very best.
Holly